Understanding Gestational Diabetes and How to Manage It
Pregnancy is transformative but can pose health challenges like gestational diabetes. Learn about its risks, diagnosis, and effective management for mother and baby's health. Read more in this article.
Pregnancy is a beautiful and transformative experience for women, but it also comes with a series of health-related challenges. One of these challenges is gestational diabetes, a condition that affects some pregnant women. Understanding gestational diabetes and learning how to manage it is crucial for the health of both the mother and the baby. In this article, we will delve into what gestational diabetes is, its risk factors, how it is diagnosed, and most importantly, how it can be managed effectively.
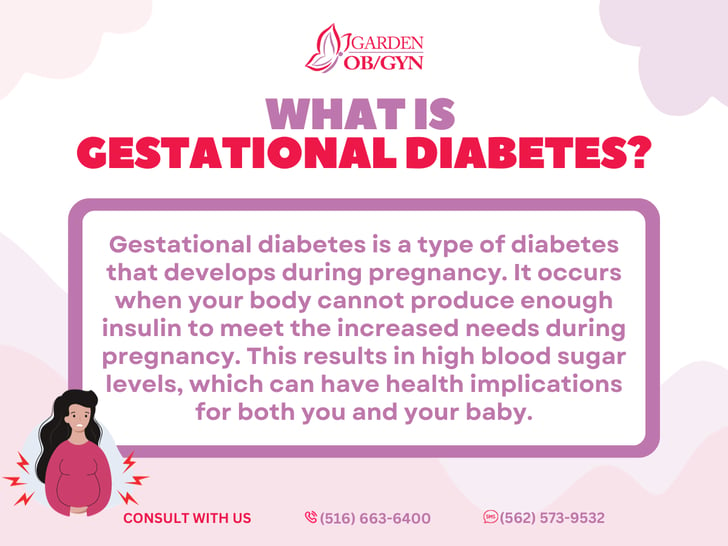
What is Gestational Diabetes?
Gestational diabetes mellitus (GDM) is a type of diabetes that occurs during pregnancy. It is characterized by high blood sugar levels that develop for the first time during pregnancy and typically resolve after childbirth. The condition arises when the body cannot produce enough insulin to meet the increased demands during pregnancy. Insulin is a hormone that regulates blood sugar levels, and when its production is insufficient, blood sugar levels can rise, leading to gestational diabetes.
Risk Factors for Gestational Diabetes
While the exact cause of gestational diabetes is not fully understood, several risk factors can increase a woman's likelihood of developing this condition during pregnancy. These risk factors include:
-
Family History: A family history of diabetes, especially among first-degree relatives (parents or siblings), increases the risk of gestational diabetes.
-
Obesity: Women who are overweight or obese before pregnancy are at a higher risk.
-
Age: Women over the age of 25 are more likely to develop gestational diabetes.
-
Previous Gestational Diabetes: Women who have had gestational diabetes during a previous pregnancy are at increased risk in subsequent pregnancies.
-
Ethnicity: Some ethnic groups, including African American, Hispanic, Native American, and Asian American, have a higher risk of gestational diabetes.
-
Polycystic Ovary Syndrome (PCOS): Women with PCOS are more prone to developing gestational diabetes.
-
High Blood Pressure: Preexisting high blood pressure can increase the risk.
Diagnosis of Gestational Diabetes
Gestational diabetes is typically diagnosed between the 24th and 28th weeks of pregnancy. The diagnosis is made through a glucose tolerance test, which involves the following steps:
-
Fasting Blood Sugar Test: The pregnant woman is asked to fast overnight, and then a blood sample is taken in the morning to measure fasting blood sugar levels.
-
Oral Glucose Tolerance Test (OGTT): After the fasting test, the woman drinks a glucose solution, and blood sugar levels are tested at specific intervals over the next few hours.
If one or more of the blood sugar measurements are higher than the recommended thresholds, a diagnosis of gestational diabetes is made.
Managing Gestational Diabetes
Effective management of gestational diabetes is essential for the health of both the mother and the baby. Fortunately, with proper care and lifestyle modifications, most women can successfully manage their blood sugar levels during pregnancy. Here are some key strategies for managing gestational diabetes:
-
Dietary Changes: A registered dietitian can help create a personalized meal plan that controls blood sugar levels. This often involves monitoring carbohydrate intake and choosing complex carbohydrates that have a slower impact on blood sugar.
-
Regular Physical Activity: Moderate and consistent exercise, such as walking or swimming, can help regulate blood sugar levels. However, it's important to consult with a healthcare provider before starting any new exercise regimen during pregnancy.
-
Frequent Blood Sugar Monitoring: Regularly checking blood sugar levels at home helps track progress and make necessary adjustments to the treatment plan.
-
Insulin or Medication: In some cases, dietary and lifestyle changes may not be enough to manage gestational diabetes, and insulin or other medications may be prescribed by a healthcare provider.
-
Prenatal Care: Regular prenatal check-ups are crucial to monitor both the mother's and the baby's health. These appointments provide an opportunity to discuss any concerns and make necessary adjustments to the treatment plan.
-
Stress Management: High stress levels can affect blood sugar control. Techniques such as deep breathing, mindfulness, and relaxation exercises can help manage stress during pregnancy.
Gestational diabetes can be a challenging condition to manage during pregnancy, but with the right guidance and support, most women can successfully control their blood sugar levels. It's essential for pregnant women to work closely with their healthcare providers, including obstetricians, dietitians, and diabetes educators, to create an individualized treatment plan. By following a balanced diet, staying active, and monitoring blood sugar levels, women with gestational diabetes can protect both their health and the health of their developing baby, ensuring a safe and healthy pregnancy experience.