Why Consider In Vitro Fertilization
IVF revolutionizes reproductive medicine, offering hope to couples struggling with natural conception. This assisted reproductive technology involves fertilizing an egg and sperm outside the body before transferring the embryo. Success depends on careful consideration of factors, guiding the decision-making process for hopeful individuals or couples.
In vitro fertilization (IVF) has revolutionized the field of reproductive medicine, offering hope to couples facing challenges in conceiving naturally. IVF involves combining an egg and sperm outside the body in a laboratory dish before transferring the fertilized embryo into the uterus. While it has proven successful for many, it is essential to carefully consider when to embark on the IVF journey. Various factors contribute to the decision-making process, and understanding them is crucial for individuals or couples contemplating this assisted reproductive technology.
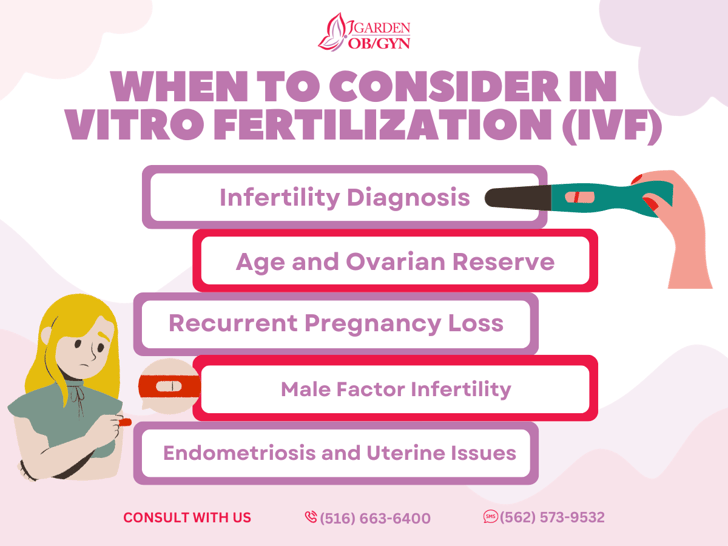
- Infertility Diagnosis:
IVF is often recommended when a couple experiences infertility issues that cannot be resolved through other fertility treatments. Infertility may result from factors such as blocked fallopian tubes, low sperm count, ovulation disorders, or unexplained fertility problems. If traditional methods like medication, surgery, or intrauterine insemination (IUI) have not yielded success, IVF becomes a viable option.
- Age and Ovarian Reserve:
A woman's age is a significant factor in fertility, and as age increases, the quantity and quality of eggs tend to decline. Women over the age of 35 may find it more challenging to conceive naturally, and IVF can be particularly beneficial in such cases. Assessing ovarian reserve through tests like anti-Müllerian hormone (AMH) and follicle-stimulating hormone (FSH) can help determine the quantity and quality of eggs, guiding the decision-making process.
- Recurrent Pregnancy Loss:
Couples who have experienced recurrent pregnancy loss may turn to IVF to increase the chances of a successful pregnancy. By closely monitoring embryos in a laboratory setting, embryologists can identify potential issues that might contribute to repeated miscarriages. Preimplantation genetic testing (PGT) can be incorporated into the IVF process to screen embryos for chromosomal abnormalities, reducing the risk of miscarriage.
- Male Factor Infertility:
When male factor infertility, such as low sperm count or motility issues, is identified, IVF with intracytoplasmic sperm injection (ICSI) may be recommended. ICSI involves injecting a single sperm directly into an egg, overcoming certain male fertility challenges. This method can be particularly effective in cases where conventional methods of fertilization may not succeed.
- Endometriosis and Uterine Issues:
Women with conditions like endometriosis, uterine fibroids, or abnormalities may opt for IVF when these issues significantly impact fertility. IVF allows for the selection of the healthiest embryos, increasing the likelihood of successful implantation and reducing the impact of uterine conditions on conception.
Deciding when to consider in vitro fertilization is a complex and personal choice. It involves a thorough evaluation of the specific fertility challenges faced by the individual or couple. Consulting with a fertility specialist, undergoing comprehensive diagnostic tests, and understanding the potential benefits and risks of IVF are crucial steps in the decision-making process. While IVF has provided hope and success to many, it is essential to approach it as one option in a broader spectrum of fertility treatments, with the ultimate goal of helping individuals and couples achieve their dream of parenthood.